Port City Critical Care Spotlight: Hi-Flow Oxygen Therapy
Oxygen therapy in veterinary medicine has remained unchanged for decades. Traditional methods of oxygen supplementation, such as flow-by, nasal prongs/cannulas, and oxygen hoods/cages, have been the mainstay for patients suffering from respiratory distress. Though these methods can deliver oxygen concentrations ranging from 20-80%, they suffer from a variety of shortcomings that can lead to treatment failure in patients with moderate to severe respiratory disease.
Mechanical Ventilation
Historically, patients failing traditional oxygen therapy were candidates for mechanical ventilation (MV). This allowed for delivery of 100% oxygen, as well as positive pressure ventilation. However, ventilation is a costly and labor-intensive process. Furthermore, mechanical ventilation itself can lead to atrophy of the breathing muscles and progressive lung trauma, known as ventilator induced lung injury (VILI).
Non-Invasive Ventilation
The desire to provide some of the benefits of mechanical ventilation while limiting the risks to patients has led to the advent of non-invasive ventilation (NIV) techniques, such as continuous positive airway pressure (CPAP), Bilevel Positive Airway Pressure (BiPAP), and hi-flow oxygen nasal cannula (HFNC) oxygen therapy. All three techniques have been described in veterinary medicine, however due to issues relating to patient comfort and equipment availability, CPAP and BiPAP have not been universally accepted. HFNC however, has been better tolerated by small animals, and as a result, is growing in popularity.
Hi-flow oxygen nasal cannula (HFNC)

Figure 1. HFNC Vapotherm unit
HFNC is more complex than an oxygen line connected to an in-line bubble-type humidifier. An HFNC unit can deliver heated and humidified oxygen titrated from 21-100% oxygen at flow rates ranging from 5-40 LPM to awake patients (Figure 1). This therapy is delivered to the patient via soft silicone binasal prongs.
HFNC has been used for the past two decades in human medicine with success. Over the past five years, this technology has been increasingly adopted in veterinary medicine, as well, and the positive effects on patient care and outcome have been increasingly noted.
The freedom of higher flow rates and oxygen concentrations provides patients with a number of physiological benefits that can be remembered with the HI-FLOW mnemonic below.
Proposed Benefits of HFNC
H: Heated and humidified air: Allows for patient comfort, reduces work to warm air while also improving laminar airflow, improves airway defenses.
I: meets patients’ Inspiratory demands: In comparison to other methods of NIV or MV, the high flow rates (up to 40 LPM) decrease work of breathing; also limits oxygen dilution with traditional methods.
F: increased Functional residual capacity (FRC): Increases in flow can increase intrathoracic pressures, which can help to recruit airflow to previously collapsed sections of lung, reversing hypoxic pulmonary vasoconstriction and improving V/Q mismatch.
L: Lightweight apparatus: The minimal weight compared with many other methods of O2 delivery allow for greater patient comfort, translating directly to decreased sedation and allowing patient mobility/respiratory physiotherapy.
O: reduced Oxygen dilution: High airflow rates lead patients to breathe in all HFNC supplied oxygen. This leads to greater alveolar oxygen concentrations than supplied by traditional oxygen methods.
W: Washout of dead space: Pharyngeal dead space accounts for a significant portion of total dead space in the conducting airways. During pauses in breathing, HFNC washes out this dead space and replaces it with the titrated oxygen levels supplied by the HFNC.
†Modified from Dysart, K et al. Research in High Flow Therapy: Mechanisms of Action. Respiratory Medicine 2009. PMID: 19467849.
HFNC at Port City
In veterinary medicine, HFNC has been primarily used in an Emergency & Critical Care setting for patients experiencing respiratory failure. Port City Veterinary Referral Hospital is excited to be able to bring this exciting new therapy to small animal patients in the New Hampshire seacoast.
Patients who benefit from HFNC
Based on current evidence, HFNC can be considered for patients with moderate to severe respiratory distress. Examples include:
- Pneumonia
- Trauma with pulmonary contusions
- Non-cardiogenic pulmonary edema
- Mild to moderate Acute respiratory distress syndrome (ARDS)
- High risk patients requiring intensive monitoring during post-op anesthetic recovery
- Assisted recovery of patients from airway evaluation and sampling
- Management and stabilization or upper airway emergencies including brachycephalic obstructive airway syndrome (BAOS), laryngeal paralysis.
Case Study: HFNO in Action, Treatment of Respiratory Distress Following Thoracic Surgery
Petey, a 10-year old male castrated Labrador Retriever, was presented to Port City for surgical resection of a thymoma. This mass had been previously found at his annual examination, and prior to surgery, Petey had been symptomatic.
Due to local extension and adhesions of the mass, a subphrenic subtotal pericardectomy was performed, as well as a partial right cranial lung lobectomy. A unilateral right phrenic neurectomy was performed as this nerve was enveloped within the thymoma. A 12 g right-sided thoracostomy tube was placed prior to closure.
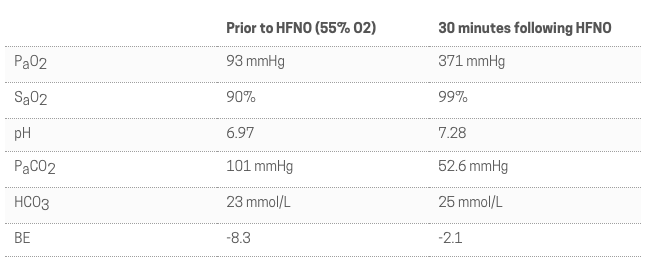
Table 1. Arterial blood gas analyses following initiation of HFNC
During anesthetic recovery, Petey developed notable respiratory distress with pulse oxygen readings between 80-85% off oxygen support. Additionally, he developed progressive hypotension that was unresponsive to fluids or vasoactive medications (dopamine, norepinephrine). Attempted supportive care measures including traditional oxygen therapy, aspiration of the chest, and augmented pain control failed to achieve respiratory and cardiovascular stability.
Based on these findings, a blood gas was performed (Table 1), which revealed a severe mixed acidosis with marked hypoventilation. Petey was suspected to have diaphragmatic dysfunction secondary to his right-sided neurectomy with concern for concurrent post-operative atelectasis and sedation, compounding his hypoxemia and hypoventilation. Due to the degree of hypoventilation, mechanical ventilation was considered based on concerns that ventilation would further hamper Petey’s respiratory muscle recovery.

Figure 2. Petey’s HFNC setup in ICU
HFNC therapy was instituted with the goal to reduce physiological dead space and enhance pCO clearance (Figure 2). After 15 minutes of HFNC therapy, Petey’s respiratory rate and effort had normalized. After 30 minutes of therapy, his blood pressure was again readable. At that time a repeat blood gas was performed (Table 1), which revealed marked improvement in his acidosis with near complete normalization of the pCO2.
Petey was maintained in hospital for six days post operatively for continued supportive care. Three days post operatively Petey was liberated from HFNC. He was then maintained in hospital for three days for continued monitoring with IV fluids, pain medications, and respiratory physiotherapy. Following discharge, Petey has recovered well at home and continues to remain very active.
 If you have cases of respiratory distress that you feel would benefit from this or other advanced respiratory therapy, please feel free to contact me and our team at Port City to discuss your case further.
If you have cases of respiratory distress that you feel would benefit from this or other advanced respiratory therapy, please feel free to contact me and our team at Port City to discuss your case further.
Written by Adam Luskin, VMD, DACVECC